What is “Inguinodynia”?
A combination of the words “inguinal”, meaning groin, and “-dynia” that refers to pain, inguinodynia can simply be described as groin pain.
Postoperative inguinodynia is a situation in which groin pain starts or persists after operation in the area. It is most commonly noted after hernia repair surgeries, simply because those are the most common surgeries in the area.
Is this something that is common after hernia surgery?
Since pain is a subjective feeling, it has been difficult to accurately figure out the incidence of postoperative inguinodynia. Early studies put it at 19% of operations but recent larger and more extensive studies have shown an incidence of around 10% for laparoscopic surgeries. (Eklund et al, 2010)
Nevertheless, this is an issue that experienced surgeons have known about and are on the lookout for. Here at Chennai Hernia Centre, Dr. Rengan has more than 30 years of experience in this field and is well equipped not just to treat your hernia, but also any unexpected complications that can arise from it.
I don’t like these odds. Can I just choose not to have my hernia operated on?
This is a valid question and we understand how distressing it is to hear of the possibility of pain even after a surgery.
To start with, 10-20% of hernia surgeries is a small enough number that most patients remain unaffected and go on to lead comfortable postoperative lives. In fact, even of the small percentage that complain of pain, an even smaller group describes it as anything but mild.
Secondly, and this is the most important reason, is that when a decision to operate on a hernia has been made, even on a non-emergency basis, there is usually a very good reason for it. What this means is that if certain risk factors are being met or fast approaching, hernia surgery is an uncompromisable decision for a patient’s life and long-term health. Remember that the only definitive treatment for hernias is surgery.
Lastly, over the last couple of decades, surgeons have learnt more and more about what the causes of postoperative inguinodynia are. This puts them at a unique advantage of not just treating the problem AFTER it occurs, but even before. Even at the initial hernia repair, surgeons have an eye out for any potential risks or body factors that could put the patient at risk of developing inguinodynia.
Keeping all this in mind, it is best that patients not shy away from an essential surgery because of the fear of complications. Nevertheless, we pride on keeping a patient-first approach in our clinic and of course, no patient must be pressured to undergo a surgery without being fully comfortable with the idea. In fact, if your hernia is mild enough, we will consider deferring surgery for as long as possible as well.
What are these reasons for Postoperative Inguinodynia?
There are a number of reasons for postoperative inguinodynia. Some of these are related directly to problems from the operation like if the mesh or sutures are placed poorly, or if the spermatic cord in the region has been affected. These can cause pain by themselves or by impinging on a nerve. Nerves can also be affected by an excessive scarring response by the patient’s body. All this makes nerve injury (neuropathy) the most common basis for pain in postoperative inguinodynia.
Post-op infection of the wound or mesh, or fistulization/sinus formation also occurs in certain patients. There are also unrelated medical conditions causing inguinodynia that could be mistaken for a postoperative cause like gynecological problems or irritable bowel syndrome.
How can postoperative inguinodynia be treated?
When neuropathy occurs from the inflammation of the nerve in the area, it usually resolves itself in a couple of months.
To figure out the area affected by pain or the involved nerve, we will perform dermato-sensory mapping. Using just a simple blunt stimulator and color markers can help determine which neural skin areas were involved. This will be repeated postoperatively to check for resolution of pain.
For immediate pain control, over-the-counter pain medications might just be enough. If that is inadequate, stronger oral or injectable treatment can be prescribed. Injectable anesthetic agents or steroids do help with maintenance of pain-relief in many cases. When the anesthetic is directed onto the nerve, that procedure is called a nerve block.
Therefore, it’s only in rare cases that re-operation is necessary to look over and/or remove the mesh and the offending nerves for resolution of the pain. Reoperation can be done in a key-hole approach as well but not in all cases.
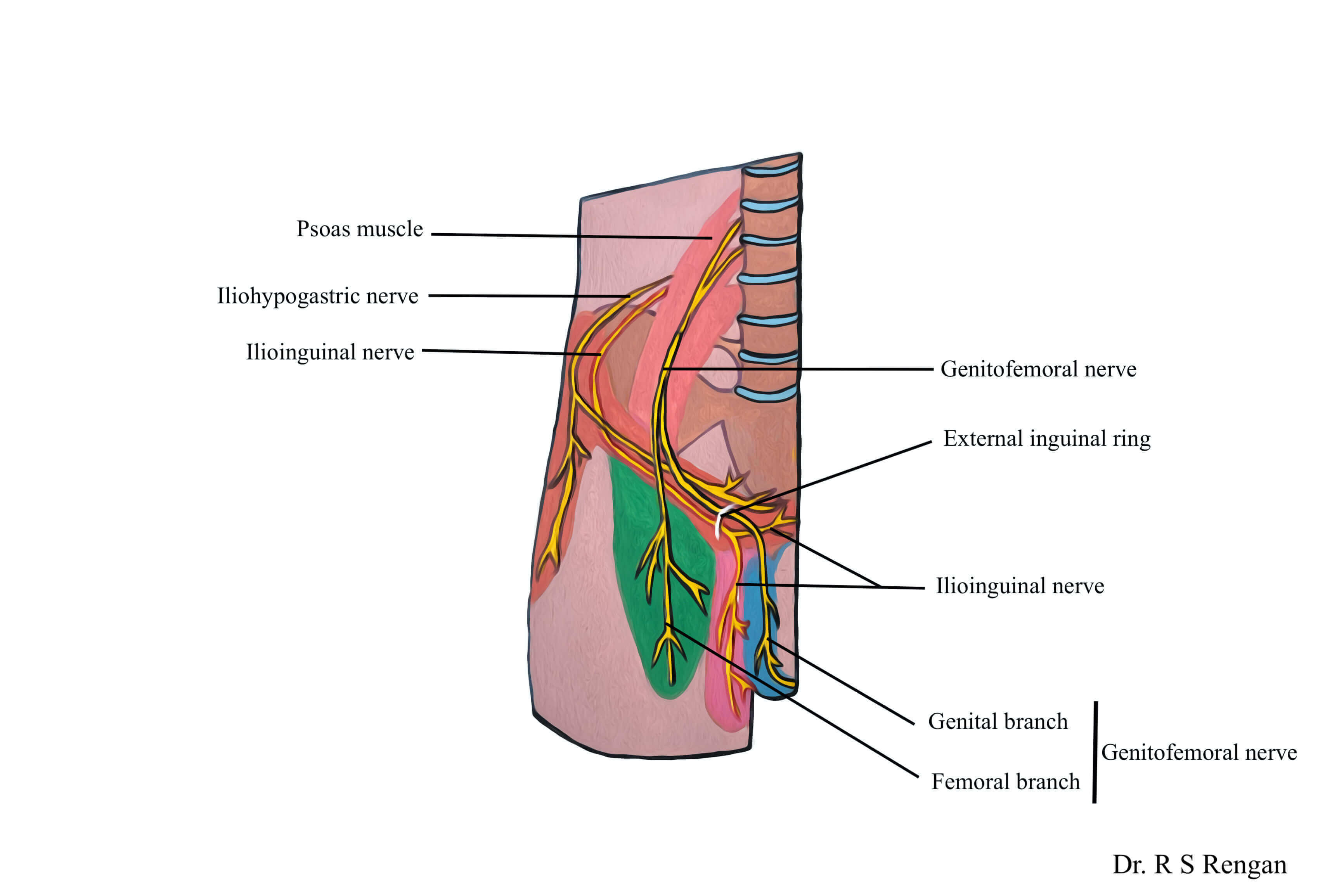
The removal of nerves is called a neurectomy. Three main sensory nerves of the groin called the ilioinguinal, iliohypogastric, and genitofemoral nerves have to be removed.
Other causes of pain like infection or misplacement have to be evaluated on a case-by-case basis, and may exist independently or in concomitance with the nerve issues. Furthermore, it is important to rule out a possibly new or previously undiagnosed condition as being the cause of this issue.
Here at Chennai Hernia Center, Dr. Rengan and his associates have had long and varied exposures to postoperative inguinodynia. They are well aware of the different causes of this condition and know how to prevent and if necessary, treat it.
